Understanding the Scope of Sports InjuriesOverview of Sports Injuries
Examples of Conditions Under Our CareCommon Sports Injuries We Treat
Clinical Assessment of Sports InjuriesHow Sports Injuries are Diagnosed
To confirm the diagnosis and evaluate the extent of the injury, the following imaging tests may be recommended:
X-ray
Identifies the location and extent of bone and cartilage damage.
CT Scan
Provides detailed cross-sectional images, especially useful for evaluating bony injuries.
MRI
Uses magnets and radio waves to create 3D images, assessing damage to ligaments, tendons, and muscles without ionizing radiation.
Arthroscopy
A minimally invasive procedure where a thin scope with a camera is inserted into the joint for inspection and potential treatment, typically done as an inpatient.
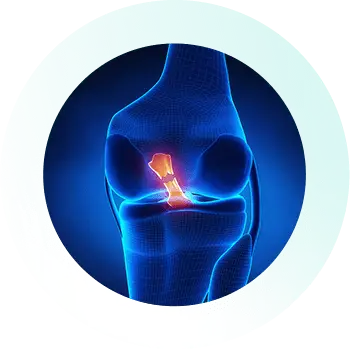
Common Sports Injuries Explained
and ACL tears, along with tips on prevention and recovery.
Overview of Sports injury Management OptionsTreatments of Sports Injuries
Non-surgical Treatments
RICE
For mild to moderate injuries, the RICE method—Rest, Ice, Compression, and Elevation—is a common first-line treatment. This approach helps reduce swelling, alleviate pain, and support the healing process for strains, sprains, and minor ligament injuries.
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen are often prescribed to manage pain and inflammation. These medications are particularly useful for conditions like tendonitis, bursitis, or soft tissue injuries.
Bracing and Support
Braces, athletic taping, or orthotics provide joint stability and reduce strain — ideal for ligament injuries, joint instability, or repetitive use conditions.
Physiotherapy
A vital part of recovery, physiotherapy involves personalized exercise programs to strengthen muscles around the injured area, improve flexibility, and enhance joint stability. It’s beneficial for recovering from tendon injuries, sprains, and post-surgical rehabilitation.
Injections
Corticosteroid and hyaluronic acid (lubricant) injections may be used for pain relief and to reduce inflammation, especially in chronic sports injuries like tendinitis or early-stage osteoarthritis.
Surgical
Treatments
Arthroscopic Surgery
This minimally invasive procedure is used to treat sports injuries with quicker recovery times. Surgeons use an arthroscope— a small camera—along with specialized instruments to access and treat joint issues such as torn meniscus or cartilage damage.
Robotic Surgery
Robotic-assisted surgical techniques offer enhanced precision during knee surgeries. This advanced technology ensures more accurate procedures, leading to faster recovery and better outcomes.
Ligament and Tendon Reconstruction
Torn ACLs, rotator cuffs, Achilles tendons, and other injuries often require reconstruction using grafts. These procedures restore joint stability and support a safe return to sport.
Cartilage Restoration Surgery
For patients with cartilage damage from sports injuries, procedures like microfracture, osteochondral grafting, or autologous chondrocyte implantation (ACI) help regenerate cartilage, reduce pain, and delay the need for joint replacement.
Replacement Surgery
For advanced sports injuries, particularly in cases of severe joint damage or degenerative conditions, total or partial knee replacement may be necessary. A total replacement involves replacing the entire joint with artificial components, while partial replacement addresses only the damaged part of the knee.
Seeking Medical Attention for Sports Injuries ConcernsWhen to See a Sports Injury Specialist
Persistent
Knee Pain
If you experience ongoing pain that doesn’t improve with rest or at-home treatments, it may be time to consult a specialist.
Swelling and Inflammation
Significant swelling, bruising, or stiffness around the injured area, particularly after physical activity, can indicate a serious sports injury.
Limited
Mobility
Struggling to bend, straighten, or bear weight on the injured joint may suggest a more severe injury that requires professional evaluation.
Injury or
Trauma
If you sustain a sports-related injury, particularly one involving a sudden twist, impact, or fall, and experience swelling or instability, seeking specialized care is important for proper recovery.
Symptoms of Arthritis
Signs like joint stiffness, swelling, and a reduced range of motion can be symptoms of sports injuries such as tendinitis or early arthritis, requiring expert treatment to prevent further damage.
Why Dr SeanSports Injury Care Backed by Performance Expertise
Your care is led by Dr. Sean Leo, a board-certified orthopaedic surgeon with over 25 years of clinical experience managing sports-related knee and lower limb injuries. His practice draws from his time with the Singapore Armed Forces and as a team physician in the New South Wales Rugby League, where he treated individuals involved in high-level physical activity.
Joint Preservation & Minimally Invasive Repair
Where suitable, Dr. Leo offers arthroscopic techniques that prioritise joint preservation and help support a return to movement.
Evidence-Based Care with a Sports Medicine Perspective
Treatment plans are structured around clinical best practices, incorporating surgical care, rehabilitation, and injury prevention strategies.
Rehabilitation Tailored to Activity Level
Dr. Leo collaborates with physiotherapists and rehab providers to develop personalised recovery plans for recreational and competitive athletes alike.
Focused Recovery Goals
The aim is to restore function, support long-term joint health, and help patients return to the activities they value most.
Expertise in
Knee & Sports Care
Evidence-Based
Practice
Care for Patient
Well-Being

Book an Appointment
Sports Injury Treatment
& Recovery FAQs
What should I do immediately after a sports injury?
If you experience a sports injury, begin with the RICE protocol (Rest, Ice, Compression, and Elevation). This helps reduce swelling and minimize tissue damage. Avoid weight-bearing if there’s pain or instability. If symptoms persist beyond 48 hours, consult a sports injury specialist for early diagnosis and faster recovery.
Do all sports injuries require surgery?
No, most sports injuries can be managed with non-surgical treatment, especially soft tissue injuries, mild sprains, and overuse conditions. Surgery may be necessary for complete ligament or tendon tears, unstable joints, or severe injuries that don’t respond to conservative care. A sports medicine doctor will recommend the best approach based on your injury and activity goals.
How long does recovery take for a sports injury?
Recovery time for sports injuries depends on the type and severity of the injury. Minor strains or sprains may heal within 1–3 weeks. Moderate injuries, such as meniscus tears or shoulder impingement, often require 6–12 weeks of rehabilitation. Major injuries like ACL tears or fractures needing surgery can take 6–12 months for full return to sport. A guided rehab plan ensures safe and effective healing.
What are the non-surgical treatment options for sports injuries?
Non-surgical sports injury treatments include physiotherapy, manual therapy, activity modification, and supportive bracing. For persistent pain or inflammation, injection therapies such as corticosteroid or PRP injections may be considered. These options help restore strength and function without the need for surgery in many cases.
Can I return to my sport after an injury and perform at the same level?
Yes, most athletes return to their sport after recovery; often stronger than before with proper rehabilitation. Return-to-sport testing ensures readiness by evaluating strength, balance, and movement mechanics. Whether it’s ACL recovery, shoulder rehabilitation, or ankle injury management, structured rehab supports full performance restoration and reduces the risk of reinjury.
How can I prevent future sports injuries?
Preventing sports injuries involves strength training, mobility exercises, and sport-specific conditioning. Proper warm-up routines, load management, and corrective techniques also play a key role. A personalized injury prevention program, guided by a physiotherapist or sports doctor, helps athletes stay active and injury-free.